How to make a health insurance claim that ensures you get back the claimed amount?
This article shows the steps to correctly file a health insurance claim so that it gets processed quickly and you get back as much as possible.
This article shows the steps to correctly file a health insurance claim so that it gets processed quickly and you get back as much as possible.
This article is a part of our detailed health insurance article series. Ensure you have read the other parts here:
This article discusses how to plan early retirement in the face of lifestyle inflation and lack of health insurance for an investor in their 40s.
This article discusses the ICICI Lombard Elevate health insurance plan to understand whether it really offers unlimited claims.
This article discusses the latest Master Circular on Health Insurance Business, issued on 29/05/2024, which introduced significant changes aimed at enhancing policyholder protection and streamlining claim settlements.
This article gives you a list of common questions and their answers on the concept of “Cashless Everywhere” introduced for health insurance.
This article talks about deductible-based health insurance plans like top-up and super-top-up and shows which one you should buy and why.
This article explains why health insurance is important, how to choose one that suits your needs, the tax benefits and where to buy it from.
This article shows you a better alternative to paying premiums every month or quarter as well as manage when premiums increase over time.
Before making a claim, it is essential to understand the role of the third-party administrator (TPA).
TPA is an intermediary who the insurance company appoints to process the claims of the insured person
The TPA takes the claim documents and other details to the insurance company for processing. However, they do not have authority over approval or rejection of the claim, which is the sole prerogative of the insurer.
If your health insurance company does not offer the services of a TPA, it means that they have an in-house claims processing team handling your claim.
There are two different types of health insurance claims. We will cover both below.
A cashless claim means you do not pay the bill or pay only a tiny part at the time of discharge from the hospital. The following conditions must be true to ensure that cashless claims are possible:
You need to locate a network hospital, typically from the list on the insurance company website or by contacting them. Ensure that you share a list of network hospitals or the process of locating one with your family if you cannot make a choice yourself.
Once admitted at the network hospital, inform the insurance company and send them a pre-authorisation form for approval. For planned procedures, you should inform the insurer before admission.
Once the hospital sends the form, it will come back as approved, and you can proceed with the treatment.
At the time of discharge, we will cover two main steps now.
You must review and authorise all bills so that you can both consent to them and pay for any items/services/expenses not covered under your policy.
The insurer will then receive the bill from the hospital and pay them directly. Since the claim is pre-approved, this process should be fast.
A reimbursement claim is one where you pay the entire bill to the hospital and then claim it from the insurer. How much of the total bill will be reimbursed will depend on the terms of the policy, hospital and procedure, level and type of service (e.g. AC/non-AC rooms), procedure type and quality of documentation.
Note: It is imperative that you, as the insured person and related family members, be either intimately familiar with the claims process or have the support of a capable TPA or health insurance agent. Being neither will lead to huge losses if the claim is not presented correctly.
A reimbursement claim, typically, will be for a procedure at a non-network hospital. This hospital selection can be involuntary, in case of an emergency where you are rushed to the nearest hospital or even by choice. Even in such cases, it is vital to inform the insurer as soon as possible.
At the time of discharge, collect the discharge summary, prescriptions and bills for submission to the insurer along with an adequately filled claim form. This vital step should be performed with adequate care and due diligence.
You need to obviously pay the entire hospital bill in full at this time to go home. Therefore a well-funded emergency fund shines here. Refill the emergency fund once you get the claim from insurance.
Once the insurance company receives the claim details, it will be processed, and they will send the amount to you by cheque or bank transfer.
Since the claim amount is reimbursement of an already occurred expense, it is tax-free in the hands of the insured person.
This situation arises when you have both covers active at a time.
If you are choosing between a corporate health cover and your personal cover for making a claim, always choose the corporate one so that no claim record in the personal cover stays intact. After all, the corporate cover will cease once you switch jobs or retire but the personal cover will stay for life.
You will be able to get good customer service as well from your company HR and the relevant TPA.
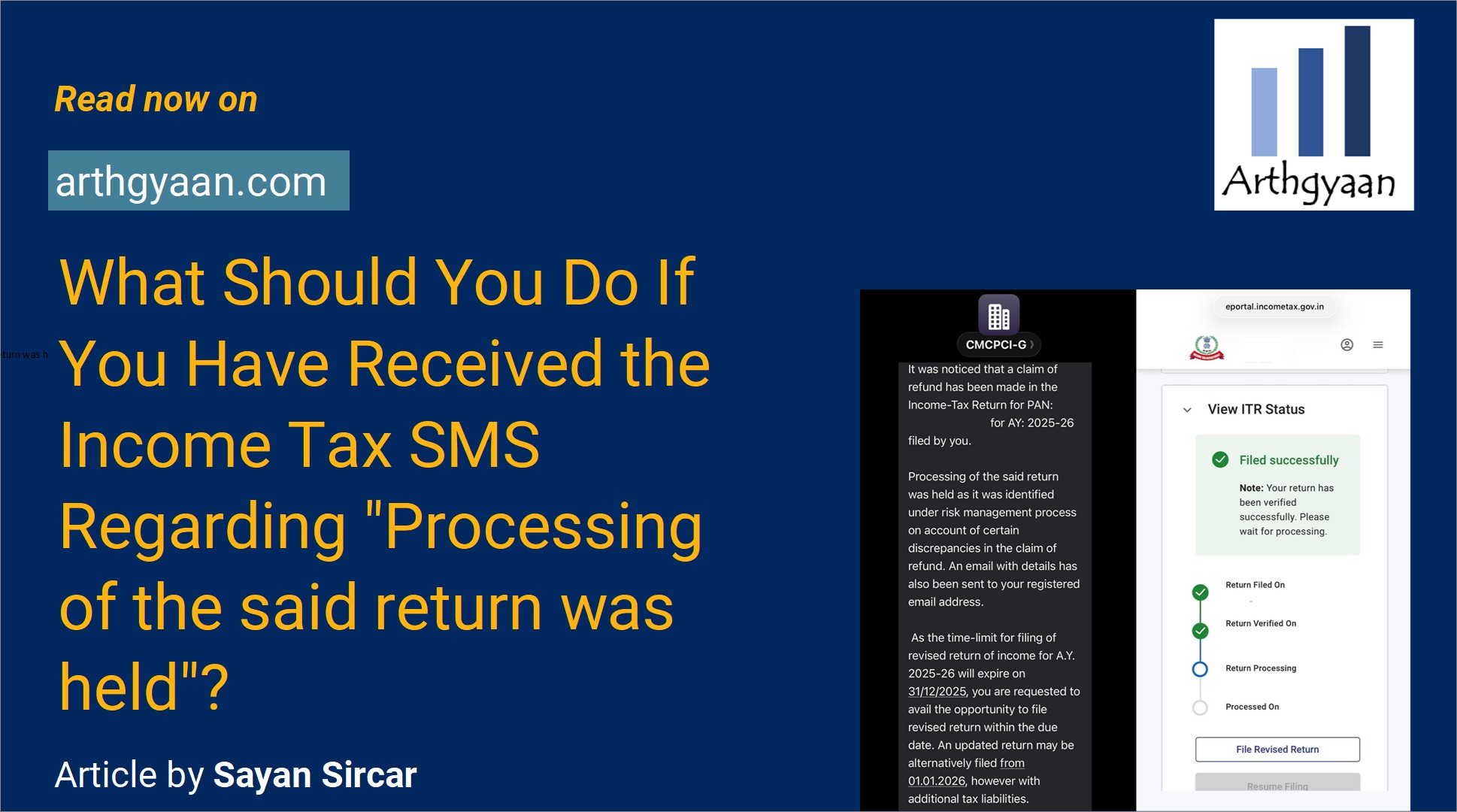
Published: 23 December 2025
6 MIN READ
Published: 18 December 2025
8 MIN READ
1. Email me with any questions.
2. Use our goal-based investing template to prepare a financial plan for yourself.Don't forget to share this article on WhatsApp or Twitter or post this to Facebook.
Discuss this post with us via Facebook or get regular bite-sized updates on Twitter.
More posts...Disclaimer: Content on this site is for educational purpose only and is not financial advice. Nothing on this site should be construed as an offer or recommendation to buy/sell any financial product or service. Please consult a registered investment advisor before making any investments.
This post titled How to make a health insurance claim that ensures you get back the claimed amount? first appeared on 21 Aug 2022 at https://arthgyaan.com
Copyright © 2021-2025 Arthgyaan.com. All rights reserved.